Multiple Sclerosis
Multiple sclerosis (MS) is a disease that occurs when the body’s immune system behaves abnormally and attacks the brain, spinal cord and optic nerves of the central nervous system (CNS). It is the leading cause of nervous system-related disability in young people, usually striking between 20 and 40 years of age.1 In the US, approximately 400,000 people have this progressive disorder, and women are two to three times more likely to develop MS than men.2,3
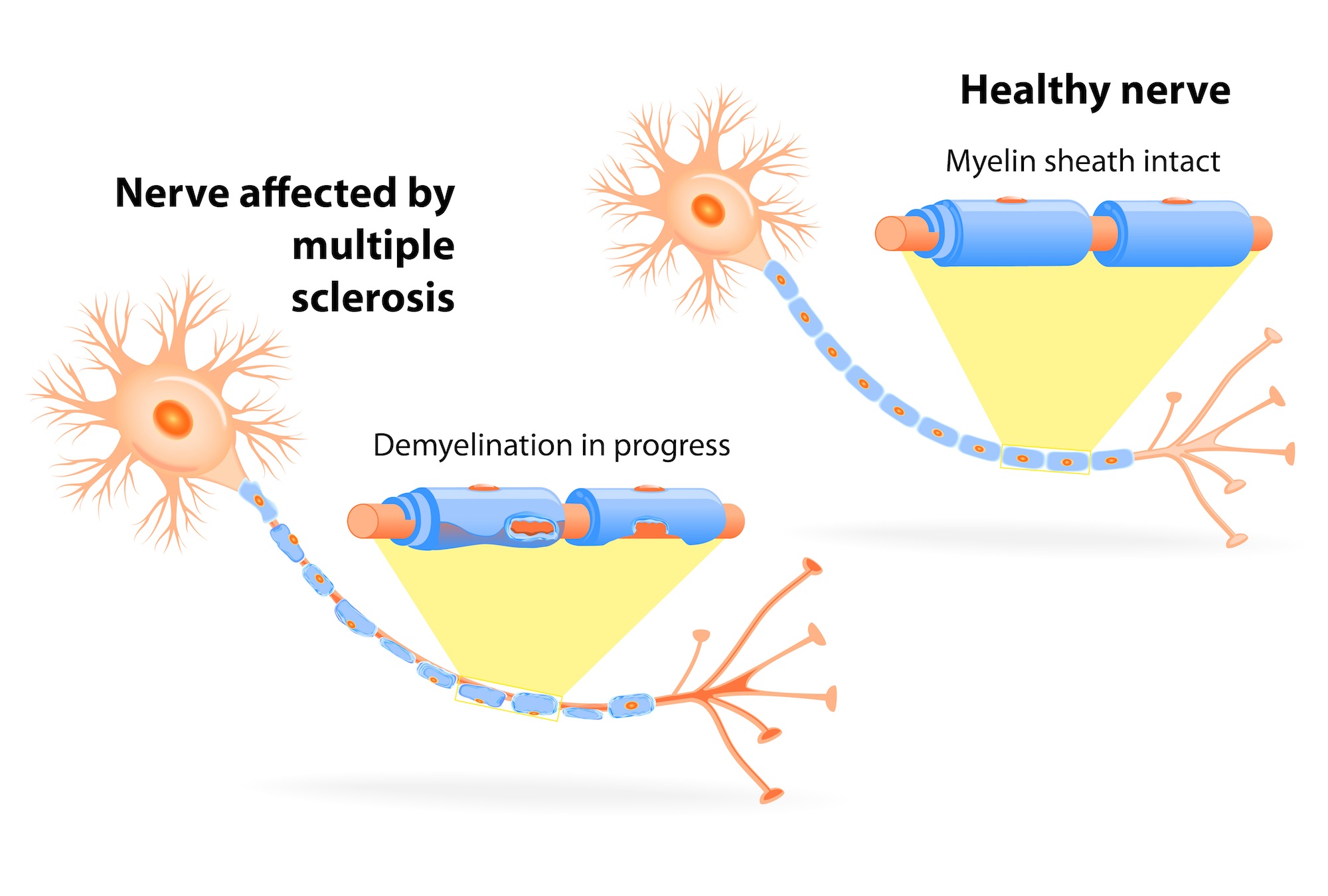
MS is a chronic disease in which the immune system attacks the myelin (the insulation around the nerves) in the brain, spinal cord and optic nerves causing inflammation and myelin damage. In people with MS, damaged nerves in the CNS lose their ability to communicate with the rest of the body, leading to unpredictable and often debilitating symptoms.4
Myelin is a fatty substance that surrounds nerves, similar to the insulation around an electrical wire. In MS, the immune system destroys the myelin and causes scarring, or sclerosis, of the nerves. This scarring interferes with the ability of nerves to conduct an electrical signal to other nerves or muscles.
What are the symptoms of MS?
Symptoms of MS vary widely from person to person. They can also change in a person over the course of the disease, temporarily disappearing or progressively worsening.5 Symptom flare-ups are known as relapses, and most people experience these during the course of the disease. The most common initial signs of MS are:3,6
- numbness
- difficulty seeing clearly or eye pain
- muscle weakness
- tingling sensations
- inability to coordinate muscle movements
Nearly 14% of people experience multiple symptoms at the onset of the disease.
As the disease progresses, people with MS may experience one or more other types of symptoms. For example, approximately 90% experience fatigue at some point. In addition:3,7,8
- >90% report loss of bladder control
- Half feel pain and abnormal sensations, such as feeling that a limb is “dead”
- Approximately 50% experience depression, although it is unknown if this mood disorder is a symptom of MS or a response to the disease
- 40-65% experience cognitive impairment, which is the leading cause of employment loss
- Later stages of the disease may be marked by partial paralysis of limbs, and most people with MS lose the ability to walk. The median time from onset of MS to severe disability is approximately 23 years
The life expectancy of people with MS may be decreased by 5-10 years.
What causes MS?
Although the cause of MS is unknown, both genetics and environment appear to contribute to risk. More than 50 genes are known to increase the risk of developing MS; none appears to have a large effect on its own.3
If a person is diagnosed with MS, the risk for their identical twin is 1 in 3 and the risk for their first cousin is 1 in 100. The risk for MS in the general population is 1 in 1,000.3
MS is more common in Caucasians and in northern countries of the world. Other environmental factors that are associated with higher risk for MS are smoking, vitamin D deficiency, and prior infection with Epstein-Barr virus.9
How is MS diagnosed?
The diagnosis of MS is complex because symptoms vary widely from patient to patient and there is no single test that confirms a diagnosis. However, doctors typically use a combination of physical examinations to identify common symptoms (e.g., abnormal movements, muscle weakness, and eye problems), followed by a scan of the CNS to identify signs of inflammation or nerve damage.3,8
Myelin damage and sclerosis can be detected using magnetic resonance imaging (MRI) in nearly all people with MS at the onset of symptoms.3,8 MRI can determine the size of damaged areas (lesions) and detect signs of active inflammation. MRI is used throughout the medical care of a person with MS to monitor disease activity and progression.
A normal brain MRI scan indicates a <20% likelihood that MS will develop. An MRI scan showing active disease and older lesions is associated with an 80% chance that MS will develop in the next 20 years.3,8
Other tests include:
- Stimulation of nerves in the CNS to measure their response time.10
- Sampling and testing cerebrospinal fluid (CSF) around the spinal cord for certain markers, although there are no definitive MS biomarkers.8
- Performing blood tests to rule out other causes of MS-like symptoms.3,8
What are the types of MS?
Although specific symptoms of MS vary among individuals, the disease usually takes one of four courses:3
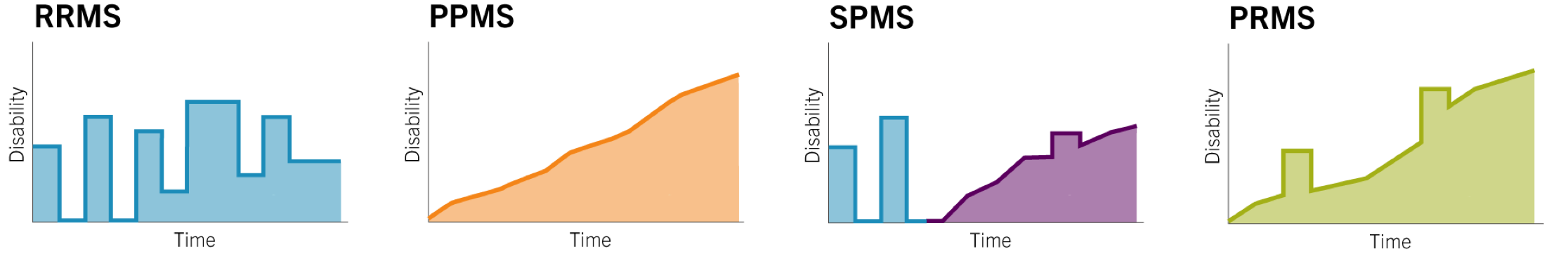
- Relapsing-remitting MS (RRMS) is the most common form of MS, with 85% of people initially experiencing episodes of acute symptoms followed by recovery periods when outward symptoms do not progress.
- Primary-progressive MS (PPMS) is a progressive form of the disease that worsens over time; however, the rate of progression is variable. The incidence of PPMS is approximately 15% of MS cases.
- Secondary-progressive MS (SPMS) is a progressive worsening of symptoms after a period of RRMS.
- Progressive-relapsing MS (PRMS) is the rarest type, marked by bouts of relapses in between progressive worsening of symptoms and only occurs in approximately 5% of people with MS.
There is increasing clinical evidence that MS progresses even when symptoms are not outwardly apparent. Newer MRI techniques and cognitive tests usually show increased disease activity, even if symptoms appear to be in remission.11 At least 90% of people with MS experience disease progression and increased disability within 20 years of onset.12
How is MS treated?
There is no cure for MS. A combination of therapies is commonly used to help people manage acute symptoms of relapse or reduce disease activity.13
- Severe relapses are treated with high-dose corticosteroids to decrease inflammation or to alleviate residual symptoms such as spasticity.
- Other residual symptoms, such as pain, may be treated with appropriate medicines.
- Rehabilitation may also be used to maintain function and ability to perform effectively at home and at work.
None of these strategies modify the disease or prevent future disability.
Several medicines have been approved by the FDA that delay disease progression in MS.13 Though progress has been made in the treatment of MS, new options are needed to help control disease activity and delay, prevent, or reverse disability.
