FDA APPROVES THE FIRST AND ONLY MEDICINE FOR CHILDREN AND ADULTS WITH ONE OR MORE FOOD ALLERGIES
February 16th, 2024
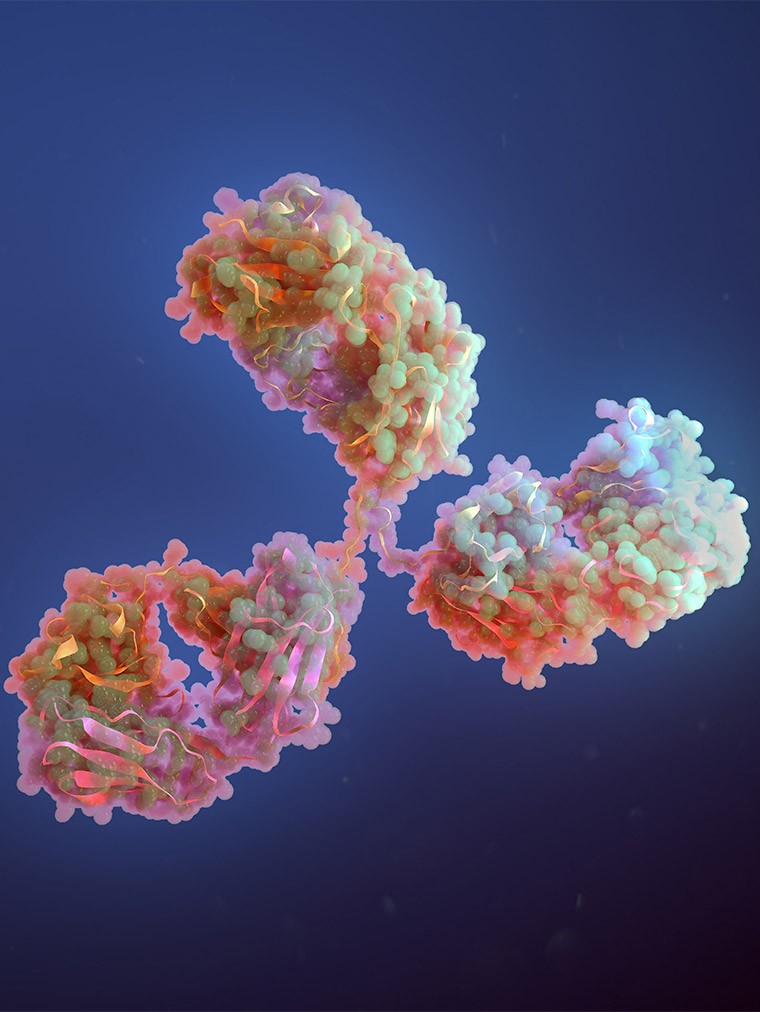
On February 16, 2024, the FDA approved Xolair® (omalizumab) for the reduction of allergic reactions, including anaphylaxis, that may occur with accidental exposure to one or more foods in adult and pediatric patients aged 1 year and older with IgE-mediated food allergy. People taking Xolair for food allergies should continue to avoid all foods they are allergic to (commonly referred to as “food allergen avoidance”). Xolair should not be used for the emergency treatment of any allergic reactions, including anaphylaxis.
News in brief
- Xolair is the first and only FDA-approved medicine to reduce allergic reactions in people with one or more food allergies.
- The approval is based on data from the NIH-sponsored Phase III OUtMATCH study, which showed a significantly higher proportion of food allergy patients as young as 1 year treated with Xolair could tolerate small amounts of peanut, milk, egg and cashew without an allergic reaction, compared to placebo.
- Immunoglobulin E (IgE)-mediated food allergies are the most common type and are typically characterized by the rapid onset of symptoms following exposure to certain food allergens.
- About 3.4 million children and 13.6 million adults in the United States have been diagnosed with IgE-mediated food allergies, based on estimates for 2024.
- Safety findings were consistent with the known safety profile of Xolair across its additional indications and in previous clinical trials.
Supporting Information

“Xolair offers patients and families an important new treatment option that can help redefine the way food allergies are managed and reduce the often-serious allergic reactions that can result from exposure to food allergens. Today’s approval builds on 20 years of patient experience and an established efficacy and safety profile since Xolair was first approved in allergic asthma. We look forward to bringing this treatment to the food allergy community who have long awaited an advancement.”